Secondo i Centri per il controllo e la prevenzione delle malattie (CDC) degli Stati Uniti, gli uomini gay, bisessuali e altri uomini sessualmente attivi che hanno rapporti sessuali con altri uomini – Gli MSM corrono un rischio maggiore di contrarre un'infezione sessualmente trasmissibileSi dice che la sifilide sia più comune tra gli uomini che trasmettono sesso (MSM) e che più della metà dei nuovi pazienti con HIV diagnosticati siano uomini che trasmettono sesso (MSM). Questa crescente epidemia di MST tra persone omosessuali è il motivo per cui la consapevolezza sulle MST è fondamentale per gli uomini che trasmettono sesso (MSM).

In questo articolo parleremo delle malattie sessualmente trasmissibili più comuni nelle comunità gay e MSM, dei segni e dei sintomi, delle pratiche di prevenzione, delle procedure di test essenziali e delle tecniche efficaci di notifica al partner.
Le malattie sessualmente trasmissibili più comuni nei rapporti gay/MSM
Per gli omosessuali/MSM, le infezioni sessualmente trasmissibili più comuni sono la sifilide, l'HIV, la gonorrea e l'herpes.
- Sifilide
La sifilide è al primo posto nella lista delle malattie sessuali gay più comuni. È un'infezione batterica causata da Treponema pallido, che si trasmette durante i rapporti sessuali anali o orali non protetti e può causare gravi problemi di salute.
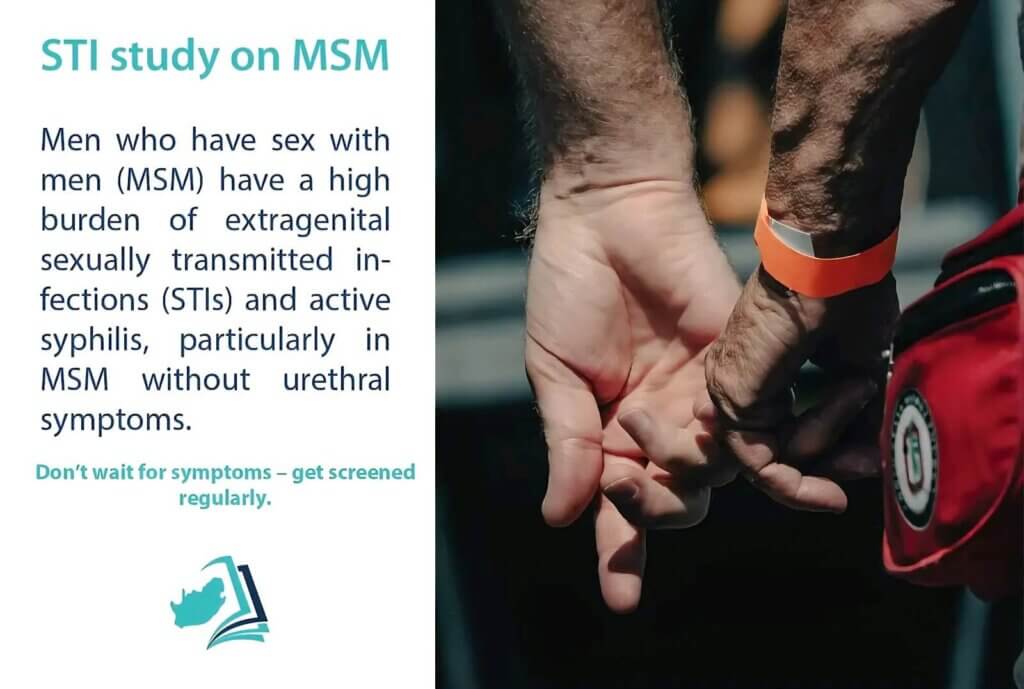
I risultati di uno studio condotto dalla London School of Hygiene and Tropical Medicine (LSHTM) in collaborazione con l'Organizzazione Mondiale della Sanità (OMS) mostrano che Gli MSM hanno un alto tasso di infezione da sifilide.
💊Sintomi
- Ulcera genitale indolore
- Eruzioni cutanee sul corpo
- ghiandole gonfie
- Ulcera della bocca
- Perdita di capelli a chiazze
❇️Misure preventive
- Uso del preservativo
- Evitare di condividere giocattoli sessuali
- Utilizzo di dighe dentali durante il sesso orale
- HIV
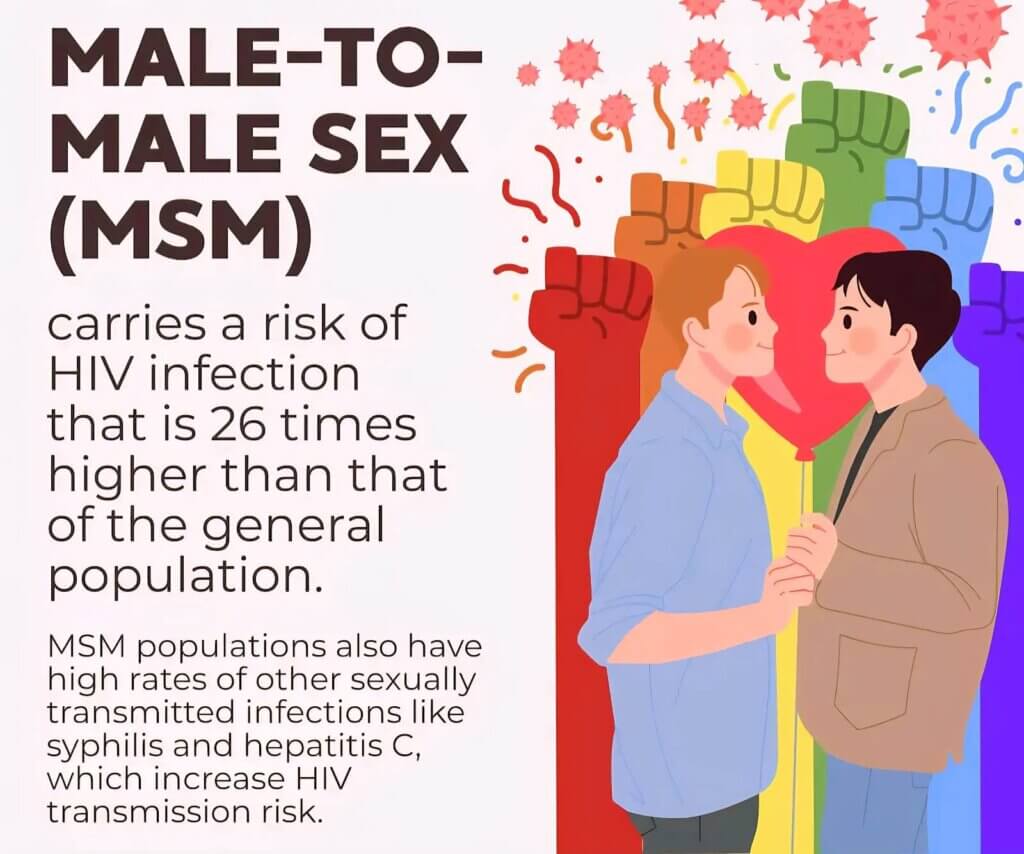
Un'altra MST associata al sesso tra uomini (MSM) è l'infezione da virus dell'immunodeficienza umana (HIV), il virus che causa la sindrome da immunodeficienza acquisita (AIDS).
L'HIV può essere trasmesso attraverso il sangue e i fluidi corporei sessuali durante il sesso orale e anale tra uomini che hanno rapporti sessuali con altri uomini. Secondo l'OMS, il rischio di contrarre l'HIV è 26 volte più alto tra gli MSM rispetto alla popolazione mondiale.
💊Sintomi
- Febbre
- dolori muscolari
- Perdita di peso
- Diarrea
- Sudorazioni notturne
❇️Misure preventive
- Uso corretto e coerente del preservativo durante i rapporti sessuali
- Evitare di condividere aghi, siringhe o altri oggetti appuntiti
- Uso di farmaci per la profilassi pre-esposizione (PrEP)
- Gonorrea
Si tratta di un'altra comune infezione sessuale tra gli MSM, che causa dolore e incapacità di urinare. Si trasmette durante i rapporti sessuali con una persona infetta.
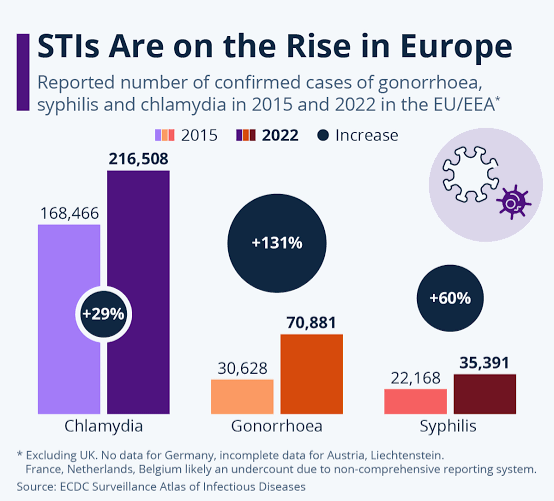
Secondo il centro per la prevenzione e il controllo delle malattie, Gli uomini che hanno rapporti sessuali con uomini hanno segnalato casi di gonorrea molto più alti rispetto agli uomini eterosessualiInoltre, i dati che mostrano un aumento delle malattie sessualmente trasmissibili in Europa negli ultimi tempi mostrano che la gonorrea ha avuto l'aumento più elevato (+131%).
💊Sintomi
- Dolore testicolare
- Dolore durante la minzione
- secrezione colorata dal pene
- Mal di gola
- prurito anale
❇️Misure preventive
- Uso del preservativo e della diga dentale
- Limitare i partner sessuali
- Non fare sesso con qualcuno che mostra sintomi di gonorrea
- Herpes
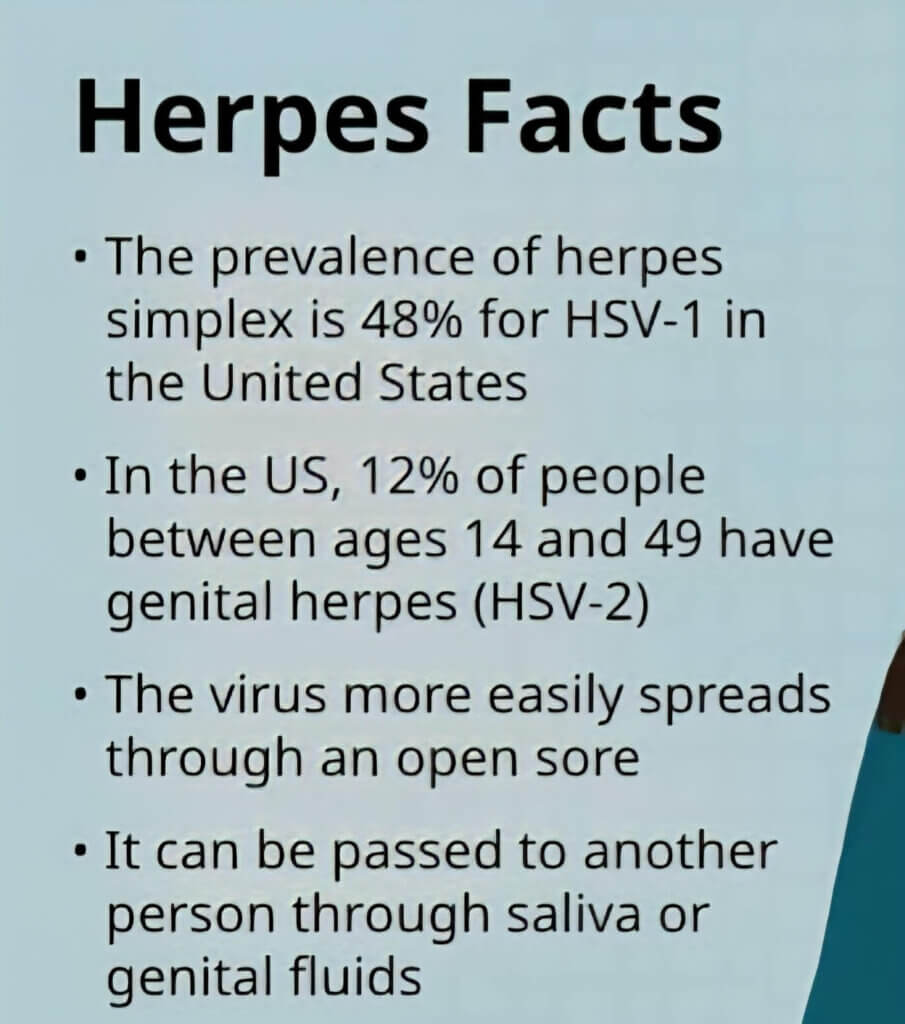
Si tratta di un'altra MST comune tra gli omosessuali, causata dal virus herpes simplex (HSV) di tipo 1 (herpes orale) e di tipo 2 (herpes genitale). L'herpes si trasmette attraverso rapporti sessuali orali, anali o contatti genitali.
I dati sull'herpes, come indicato, mostrano che il 48% delle persone negli Stati Uniti convive con l'herpes orale, mentre il 12% delle persone di età compresa tra 14 e 49 anni soffre di herpes genitale. Gli MSM rappresentano la percentuale più alta di infezioni da herpes genitale (48,9%).
💊Sintomi
- Vesciche o piaghe dolorose sui genitali
- Sensazioni di bruciore nella zona genitale
- Prurito
- Febbre
- Mal di testa
❇️Misure preventive
- Limitare i partner sessuali
- Uso costante di preservativi e dighe dentali
- Non condividere i giocattoli sessuali
Segni chiave delle malattie sessualmente trasmissibili negli uomini gay
I segni e i sintomi delle malattie sessualmente trasmissibili potrebbero non essere evidenti immediatamente dopo aver contratto l'infezione. Infatti, la persona infetta potrebbe non manifestare alcun sintomo evidente (asintomatico). Pertanto, se sei gay o MSM sessualmente attivo, è necessario sottoporsi spesso al test.
👉Sebbene i principali segnali di MST negli uomini gay che possono essere notati dopo un po' di tempo (circa 20 giorni) includono:
- Piaghe e protuberanze genitali.
- Eruzioni cutanee
- Vesciche.
- Dolore o prurito nella zona del pene o dell'ano.
- Scolorimento della pelle del pene o dell'ano.
- Dolore durante la minzione o l'eiaculazione.
- Aumento della frequenza della minzione.
- Perdite colorate e maleodoranti dal pene o dall'ano.
- Febbre.
- Fatica.
- Gonfiore dei linfonodi.
- Sanguinamento dall'ano o dal pene.
- Ingiallimento della pelle o degli occhi.
- Dolore e gonfiore dei testicoli.
- Mal di testa e dolori muscolari.
Test essenziali per le malattie sessualmente trasmissibili (IST) per gli uomini con MSM
Gli ultimi Rapporti Epidemiologici Annuali sulle MST pubblicati dall’ECDC (Centro Europeo per la Prevenzione e il Controllo delle Malattie) affermano che I casi di malattie sessualmente trasmissibili continuano ad aumentare in tutta Europa. Gli studi hanno anche dimostrato storicamente che i tassi più elevati di malattie sessualmente trasmissibili si sono verificati tra gli uomini che vivono con gli uominiPertanto, per prevenire un'ulteriore trasmissione e ridurre l'impatto delle malattie sessualmente trasmissibili sulla salute pubblica, è necessario aumentare i test per le malattie sessualmente trasmissibili tra gli uomini che hanno rapporti sessuali con altri uomini.
Come sottoporsi al test
- Visitare una clinica o un centro sanitarioContatta e informati sui servizi di qualsiasi clinica o centro sanitario specializzato in malattie sessualmente trasmissibili (IST) nella tua zona. Successivamente, puoi prenotare un appuntamento.
- Parlane con il tuo medico: Informa il tuo medico o il tuo operatore sanitario dei tuoi problemi di MST e discuti con lui/lei della tua storia sessuale. Sono nella posizione migliore per fornirti una Guida al test per le malattie sessualmente trasmissibili per te e consigliarti sulle opzioni di trattamento o gestione disponibili.
- Seguito: Dopo aver ricevuto il risultato del test per le malattie sessualmente trasmissibili (positivo o negativo), assicurati di contattare il tuo medico o l'operatore sanitario per ulteriori istruzioni.
- Seguire attentamente le istruzioni per i test dei kit casalinghi: Se si sceglie di utilizzare kit per il test casalingo per le malattie sessualmente trasmissibili (IST) come gonorrea, HIV, sifilide e clamidia, assicurarsi di seguire scrupolosamente le istruzioni del kit per evitare risultati falsi.
Dove fare il test
Ecco un elenco di posti dove puoi ottenere un Test e trattamento delle malattie sessualmente trasmissibili in Australia, Europa e altre parti del mondo.
- Cliniche per la salute sessuale: Puoi rivolgerti a qualsiasi clinica per la salute sessuale specializzata in test e trattamenti per le malattie sessualmente trasmissibili. Sono accessibili a tutti, indipendentemente da età, sesso o orientamento sessuale. Alcuni esempi sono le cliniche per la salute sessuale di Greenwich e del Servizio Sanitario Nazionale del Regno Unito.
- Centri di pianificazione familiare: Spesso, i centri di pianificazione familiare offrono servizi di test e trattamento per le malattie sessualmente trasmissibili. Puoi rivolgerti a chiunque ti sia vicino.
- Centri sanitari comunitari: La maggior parte delle organizzazioni o dei centri comunitari offrono servizi di analisi e cura delle malattie sessualmente trasmissibili a prezzi accessibili.
- Organizzazioni sanitarie controllate dalla comunità aborigena (ACCHO): Queste organizzazioni forniscono test per le malattie sessualmente trasmissibili culturalmente sicuri nelle comunità locali.
Notifica al partner: un passaggio fondamentale
Se il test è positivo, il passo successivo è informare il/i partner. Questo passaggio è essenziale perché aiuta a prevenire ulteriori contagi e complicazioni. Come affermato in precedenza, alcune malattie sessualmente trasmissibili (MST) tra gli omosessuali sono asintomatiche, quindi è meglio informare il/i partner in modo che possano sottoporsi al test e curarsi.
I metodi tradizionali di notifica al partner (che prevedono che tu o il tuo medico informiate direttamente il vostro partner) possono essere difficili da attuare. Alcuni dei motivi per cui possono essere difficili da attuare sono: potenziale disagio, stigmatizzazione, paura di conseguenze negative e risorse di comunicazione inadeguate (per i servizi sanitari o le cliniche).
La soluzione più efficace per la notifica ai partner diventa quindi l'uso di servizi di notifica STI anonimi come Anonimi TellYourPartnerTi aiuta a inviare messaggi di testo sulle malattie sessualmente trasmissibili (IST) al tuo partner in modo semplice, completo e gratuito, in modo anonimo. Oltre all'anonimato, il fatto che possa inviare messaggi a più destinatari contemporaneamente è il motivo per cui è un'ottima scelta per gli MSM (che a volte hanno più partner sessuali).
👉Segui questi semplici passaggi:
- Vai al Anonimi TellYourPartner sito web e clicca su Avvisare un partner.
- Seleziona l'infezione sessualmente trasmissibile per cui sei risultato positivo.
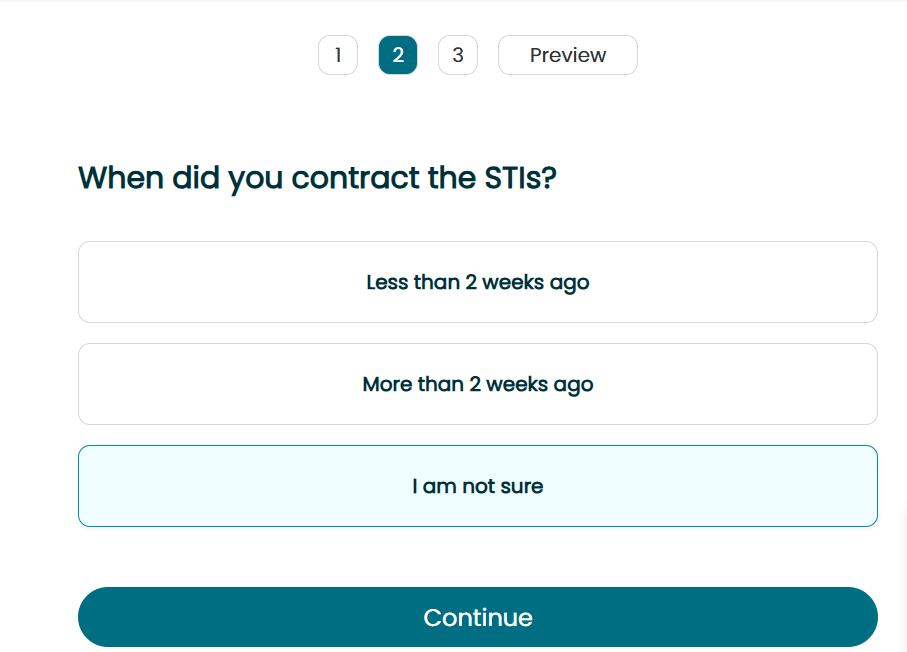
- Seleziona il momento in cui hai contratto la MST.
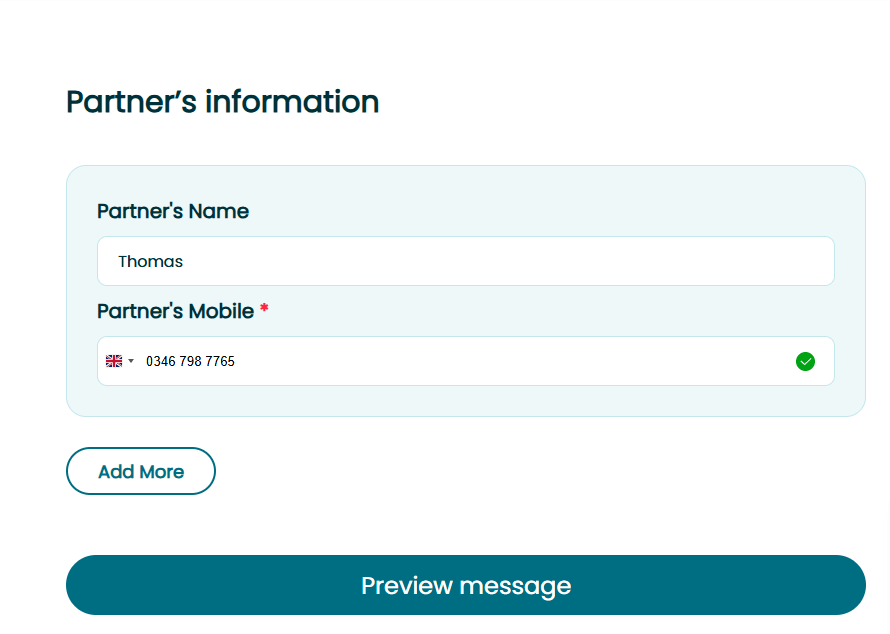
- Inserisci le informazioni del tuo partner (nome e numero di telefono). Fai clic Aggiungi altro per inviare a più destinatari.
- Clic Anteprima messaggio per vedere il messaggio che verrà inviato.
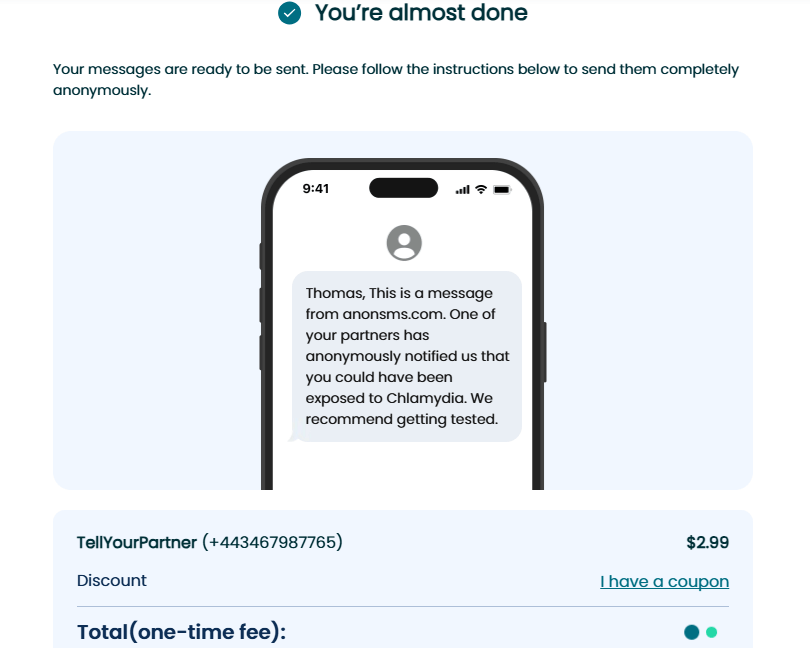
- Effettua il pagamento e invia.
Prevenzione delle malattie sessualmente trasmissibili per uomini con disabilità (MSM) Sesso e risorse
Le misure illustrate di seguito possono aiutare a ridurre il rischio di contrarre una MST per gli MSM.
- Usa il preservativo: L'uso corretto e costante di preservativi e dighe dentali durante i rapporti sessuali anali o orali riduce efficacemente il rischio di trasmissione di malattie sessualmente trasmissibili.
- Vaccinazione: La vaccinazione può proteggerti dalle malattie sessualmente trasmissibili come l'epatite A, l'epatite B e l'HPV.
- PrEP (Profilassi pre-esposizione): La PrEP prevede l'assunzione di farmaci come Truvada, Descovy e Apretude prima del rapporto sessuale per prevenire l'infezione da HIV bloccando il ciclo vitale del virus.
- Doxy PEP (profilassi post-esposizione alla doxiciclina): Questi farmaci possono aiutare a prevenire lo sviluppo di malattie sessualmente trasmissibili (IST) batteriche, come la gonorrea e la sifilide. Devono essere assunti 24-72 ore dopo il rapporto sessuale.
- Soci limitanti: È possibile ridurre il rischio di esposizione alle malattie sessualmente trasmissibili riducendo il numero di partner sessuali.
🌟Altre risorse utili
Siti web come www.cdc.gov, www.hiv.gov, www.naccho.org, E www.cdph.ca.gov, forniscono informazioni utili sui test, la prevenzione e il trattamento di varie malattie sessualmente trasmissibili tra gli uomini che convivono con gli uomini.
Conclusione
La prevenzione delle malattie sessualmente trasmissibili (IST) legate al sesso gay, i test e la notifica al partner sono molto importanti per prevenire un'ulteriore trasmissione e ridurre l'impatto delle IST sulla comunità gay e MSM.
Tuttavia, i metodi tradizionali di notifica ai partner possono essere difficili da attuare, quindi è meglio informarli in modo confidenziale tramite Anonsms TellYourPartner. È facile da usare, garantisce l'anonimato 100% e può essere utilizzato per inviare notifiche sulle malattie sessualmente trasmissibili a più destinatari in qualsiasi parte del mondo.
Domande frequenti sulle malattie sessualmente trasmissibili legate al sesso gay
Hai ancora domande? Qui sotto trovi le risposte ad alcune domande frequenti sulle malattie sessualmente trasmissibili legate al sesso gay.
- Quale percentuale di uomini gay ha una STl?
La percentuale di uomini gay affetti da una MST cambia di tanto in tanto. Ma gli studi hanno dimostrato che, tra tutte le popolazioni, gli uomini gay rappresentano circa il 711% dei casi di HIV e la più alta percentuale di casi di sifilide ogni anno.
- Quali test STl dovrebbero sottoporsi agli uomini gay?
Il CDC raccomanda che gli uomini gay sessualmente attivi si sottopongano al test per l'HIV, la sifilide, l'epatite B e C, la gonorrea e la clamidia.
- Quali sono i rischi del sesso gay non protetto?
I rapporti sessuali non protetti tra uomini gay aumentano il rischio di contrarre malattie sessualmente trasmissibili (MST) come HIV, clamidia, sifilide, herpes genitale e verruche, gonorrea ed epatite B.
- È più sicuro puntare in alto che in basso?
Sì, considerando il rischio di trasmissione di malattie sessualmente trasmissibili (come l'HIV), il topping (sesso anale insertivo) è considerato più sicuro del bottoming (sesso anale ricettivo).

 Anonsmi
Anonsmi
 Gentell
Gentell